Key Takeaways
- Blood in stools can be either visible (overt) or hidden (occult), and distinguishing between the two is crucial for diagnosis.
- Occult blood may indicate early gastrointestinal disease and often requires laboratory testing for detection.
- Visible blood in stools usually points to more advanced or acute conditions, such as hemorrhoids, infections, or gastrointestinal bleeding.
- Prompt medical evaluation is essential, as underlying causes can range from minor issues to serious diseases, including colorectal cancer.
Occult vs Visible: What Is the Difference?
Blood in stools can be visibly red or black, or hidden and only detectable through laboratory tests. Visible blood often indicates acute or localized bleeding, whereas occult blood may signal early disease or slow gastrointestinal bleeding, making early evaluation critical.
Understanding Blood in Stools
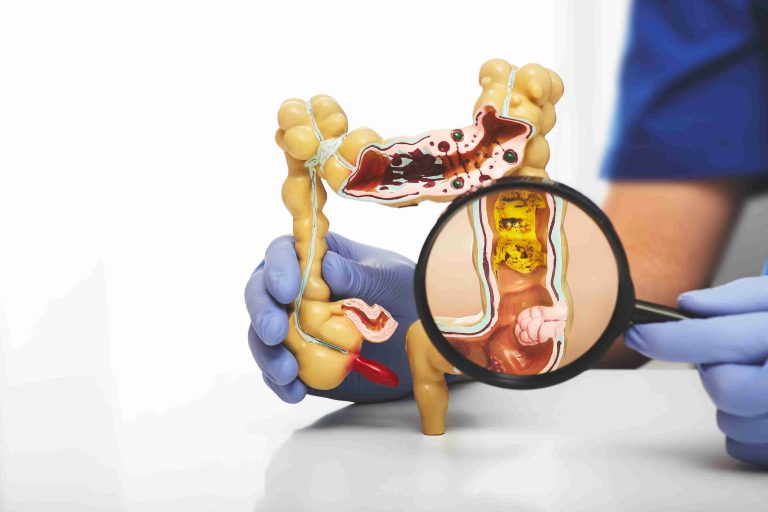
Blood in stools is a symptom that can range from alarming to subtle, depending on its appearance, amount, and frequency. The presence of blood reflects bleeding somewhere along the digestive tract, which may include the esophagus, stomach, small intestine, or colon.
Healthcare providers classify blood in stools into two main categories: visible (overt) and hidden (occult). Understanding these distinctions helps guide further testing, diagnosis, and treatment.
Occult Blood: The Hidden Threat
Occult blood refers to small amounts of blood in the stool that are not visible to the naked eye. Patients may not notice any discoloration, and the bleeding often occurs slowly or intermittently.
Detection of occult blood typically requires stool testing, such as the fecal occult blood test (FOBT) or fecal immunochemical test (FIT). These tests are especially useful in colorectal cancer screening programs and for detecting early gastrointestinal disease.
Because occult bleeding is not noticeable, patients might experience no obvious symptoms besides subtle signs such as mild fatigue or iron deficiency anemia. Recognizing this form of blood in stools is crucial for early intervention.
Visible Blood: When It’s Obvious
Visible blood in stools is also referred to as overt bleeding. This type of bleeding can appear as bright red blood on the surface of the stool, streaks mixed with stool, or dark, tarry stools in cases of upper gastrointestinal bleeding.
Causes of visible blood in stools include hemorrhoids, anal fissures, gastrointestinal infections, diverticulosis, inflammatory bowel disease, and peptic ulcers. Unlike occult blood, overt bleeding usually signals active or more advanced disease, prompting immediate medical evaluation.
Color and Characteristics Matter
The color of blood in stools helps clinicians estimate the bleeding site. Bright red blood typically originates from the lower gastrointestinal tract, such as the colon, rectum, or anus. Dark, black, or tarry stools often indicate bleeding in the upper gastrointestinal tract, including the stomach or small intestine.
Understanding the nature of blood in stools allows doctors to narrow down potential causes and prioritize diagnostic tests accordingly.
Associated Symptoms and Risk Factors
The presence of blood in stools is often accompanied by other symptoms, which can provide clues about the underlying condition. Common associated symptoms include abdominal pain, changes in bowel habits, unexplained weight loss, fatigue, or weakness from anemia.
Risk factors for gastrointestinal bleeding include a family history of colorectal cancer, long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), gastrointestinal infections, and chronic inflammatory conditions such as Crohn’s disease or ulcerative colitis.
Diagnostic Evaluation
Evaluating blood in stools begins with a thorough medical history and physical examination. Doctors inquire about the duration of bleeding, appearance of stools, accompanying symptoms, and relevant personal or family history.
For occult blood, stool tests such as FOBT or FIT are commonly used. These tests detect small amounts of hidden blood and help identify patients who need further investigation. For visible bleeding, endoscopic procedures like colonoscopy or upper endoscopy are often recommended to locate and treat the source.
Laboratory tests may include complete blood counts to assess anemia, iron studies, and in some cases, imaging studies to evaluate the gastrointestinal tract.
Treatment Based on Cause
Management of blood in stools depends on the underlying cause. Occult bleeding caused by early-stage colorectal cancer, polyps, or minor gastrointestinal lesions may require endoscopic intervention or surgical management. Lifestyle adjustments, such as dietary modifications and cessation of NSAID use, can also help prevent further bleeding.
Visible bleeding is addressed according to severity and location. Hemorrhoids or anal fissures may be treated with topical therapies, lifestyle changes, or minor procedures. More serious causes, such as ulcers, diverticular bleeding, or malignancy, may require endoscopic treatment, medications, or surgery.
When to Seek Immediate Medical Attention
Although not all instances of blood in stools are emergencies, certain warning signs necessitate urgent evaluation. These include:
- Large amounts of bright red or dark black blood in stools
- Persistent or recurrent bleeding
- Severe abdominal pain
- Dizziness, weakness, or fainting
- Unexplained weight loss or chronic fatigue
Early assessment ensures timely diagnosis and reduces the risk of complications.
Prevention and Monitoring
Regular screening for occult blood in stools is recommended for individuals above 50 years or those with risk factors for colorectal cancer. Early detection significantly improves treatment outcomes.
Lifestyle modifications, including a high-fiber diet, adequate hydration, regular exercise, and avoiding excessive NSAID use, may reduce the risk of gastrointestinal bleeding. Maintaining routine check-ups and reporting any changes in bowel habits can also help identify issues before they become severe.
Children and Special Populations
In children, blood in stools may be caused by anal fissures, infections, or dietary intolerances. While often less serious, it is important to investigate persistent bleeding to rule out more significant conditions such as inflammatory bowel disease.
Pregnant women and elderly individuals may experience subtle or atypical symptoms. Occult blood in stools in these groups may signal serious pathology, making routine screening and timely evaluation essential.
Conclusion
Both occult and visible blood in stools serve as important warning signs of gastrointestinal health issues. Occult blood is subtle and requires testing, whereas visible blood is immediately noticeable and may indicate more urgent conditions.
Recognizing the characteristics, associated symptoms, and risk factors allows patients and clinicians to differentiate between minor issues and potentially serious diseases. Prompt evaluation, early intervention, and routine screening are key to managing gastrointestinal health effectively.
By understanding these differences, individuals can take proactive steps, whether through lifestyle adjustments, preventive screening, or seeking urgent medical care. Early recognition of blood in stools—whether hidden or visible—can prevent serious complications and improve long-term outcomes.