Colorectal cancer is one of the most common cancers worldwide, but when it runs in families, the risk can be significantly higher. People with inherited genetic conditions such as Lynch syndrome or familial adenomatous polyposis (FAP) have a much greater chance of developing colorectal cancer, often at a younger age than the general population. For these high-risk individuals, regular colonoscopy screenings are a critical tool for early detection and prevention. Understanding why colonoscopy is essential for genetic cancer risks can help you take proactive steps to protect your health.
How Genetics Influence Colorectal Cancer Risk
While anyone can develop colorectal cancer, certain inherited genetic mutations dramatically increase the likelihood of it occurring. Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), is one of the most common genetic conditions linked to colorectal cancer. It is caused by mutations in DNA repair genes, leading to a lifetime risk of up to 80% for developing the disease.
Another condition, familial adenomatous polyposis (FAP), causes hundreds or even thousands of polyps to form in the colon at an early age. Without preventive measures, nearly all individuals with FAP will develop colorectal cancer, often before the age of 40. Other hereditary syndromes, such as MUTYH-associated polyposis, also increase risk.
These genetic conditions often do not show symptoms until polyps or cancer have already developed. That’s why proactive screening with colonoscopy is so important for people who know they have a family history or genetic predisposition to colorectal cancer.
Why Colonoscopy Is the Preferred Screening Method
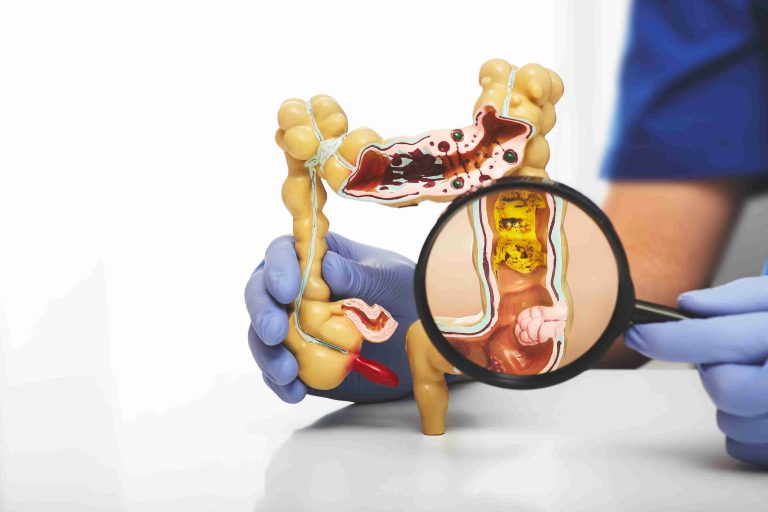
A colonoscopy is a minimally invasive procedure that allows doctors to view the entire colon and rectum using a thin, flexible tube with a camera. It is the most reliable way to detect precancerous polyps or early-stage cancers that might not be visible through other screening methods.
Unlike stool-based tests, which can only detect signs of cancer after it develops, colonoscopy can actually prevent cancer by removing polyps before they turn malignant. This makes it an especially powerful tool for people with genetic cancer risks.
During the procedure, if any abnormal growths are found, they can often be removed immediately. Tissue samples may also be taken for further testing, helping doctors determine the best management plan. For high-risk patients, this combination of detection and prevention is essential.
Earlier and More Frequent Screenings for High-Risk Individuals
For average-risk adults, colonoscopy is typically recommended starting at age 45 or 50 and repeated every 10 years. However, for those with genetic predispositions, the guidelines are much more aggressive.
Individuals with Lynch syndrome are often advised to begin colonoscopy screenings as early as age 20 to 25, with follow-up exams every one to two years. For people with familial adenomatous polyposis, screenings may start in the teenage years because polyps can form at a very young age.
This earlier and more frequent surveillance is crucial because cancers linked to genetic syndromes tend to develop more rapidly than in the general population. By catching polyps or abnormal changes early, doctors can intervene before they progress into advanced disease.
The Role of Family History and Genetic Testing
Knowing your family history is a key step in determining whether you may be at higher genetic risk for colorectal cancer. If multiple family members have had colorectal cancer or related cancers such as endometrial, ovarian, or gastric cancer, it could indicate an inherited syndrome.
Genetic testing can confirm whether you carry mutations associated with conditions like Lynch syndrome or FAP. If a mutation is identified, doctors will recommend a personalized screening plan that includes colonoscopy procedures at more frequent intervals.
Even if you test negative for a known mutation, having a strong family history may still warrant earlier or more frequent screening. Discussing your family background with a healthcare provider ensures that you receive the most appropriate guidance.
Prevention Beyond Screening
While a colonoscopy exam is the most effective way to prevent colorectal cancer in genetically predisposed individuals, it is not the only step. Maintaining a healthy lifestyle with a diet rich in fiber, regular physical activity, limited alcohol intake, and no smoking can also reduce overall cancer risk.
For some individuals with very high genetic risk, preventive surgeries such as colectomy (removal of the colon) may be recommended. This is more common in conditions like FAP where the polyp burden is extremely high and cannot be managed with regular colonoscopy alone.
Additionally, certain medications, such as aspirin or nonsteroidal anti-inflammatory drugs, may have a protective effect against polyp formation, although these should only be taken under medical supervision.
Emotional and Practical Considerations
Learning about a genetic cancer risk can be emotionally challenging. The thought of undergoing frequent colonoscopy screenings may feel overwhelming, especially at a young age. However, it is important to view these screenings as a powerful form of prevention rather than a burden.
Many people find peace of mind knowing that they are taking proactive steps to reduce their risk. Colonoscopy is a relatively quick procedure with minimal recovery time, and the reassurance it provides is invaluable. Support groups and genetic counselors can also help individuals and families cope with the emotional aspects of inherited cancer risk.
Access and Cost Considerations
For some, concerns about the cost or availability of frequent colonoscopy screenings may create hesitation. Fortunately, many health insurance plans cover colonoscopy for high-risk individuals as part of preventive care. In some regions, government screening programs also provide coverage for genetic testing and surveillance.
If cost is an issue, discussing financial assistance options with your healthcare provider or hospital can help. Many medical centers have resources to support patients who require frequent screenings due to genetic conditions.
Taking Charge of Your Health
If you have a known genetic cancer risk or a strong family history of colorectal cancer, the most important step you can take is to talk to a healthcare provider about a personalized screening plan. Colonoscopy is a critical tool for detecting and preventing cancer in high-risk individuals, and starting screenings early can truly save lives.
By staying informed about your genetic risk, keeping up with recommended colonoscopy schedules, and making healthy lifestyle choices, you can significantly reduce the likelihood of developing advanced colorectal cancer. Early detection is your best defense, and regular screening is an investment in your long-term health.
Conclusion
Colonoscopy plays an essential role in managing genetic cancer risks. For individuals with conditions like Lynch syndrome or familial adenomatous polyposis, early and frequent screenings are crucial for catching problems before they progress.
While the idea of genetic cancer risk may feel daunting, proactive screening empowers you to take control of your health. By combining colonoscopy with genetic testing, lifestyle changes, and, when needed, preventive treatments, you can greatly improve your chances of staying healthy and cancer-free.