Endoscopy is a crucial diagnostic tool used by doctors to view the internal organs and structures of the body. Whether for detecting disease, identifying abnormalities, or assessing treatment progress, it serves as a non-invasive procedure that provides detailed, real-time images.
Among the many types of endoscopic procedures, upper endoscopy (also known as esophagogastroduodenoscopy or EGD) and lower endoscopy (often referred to as colonoscopy) are the two most commonly performed.
While both involve the use of a flexible tube with a camera, they focus on different areas of the gastrointestinal (GI) tract. Understanding when each procedure is needed and how they differ is crucial in making informed decisions about your health.
What is Endoscopy?
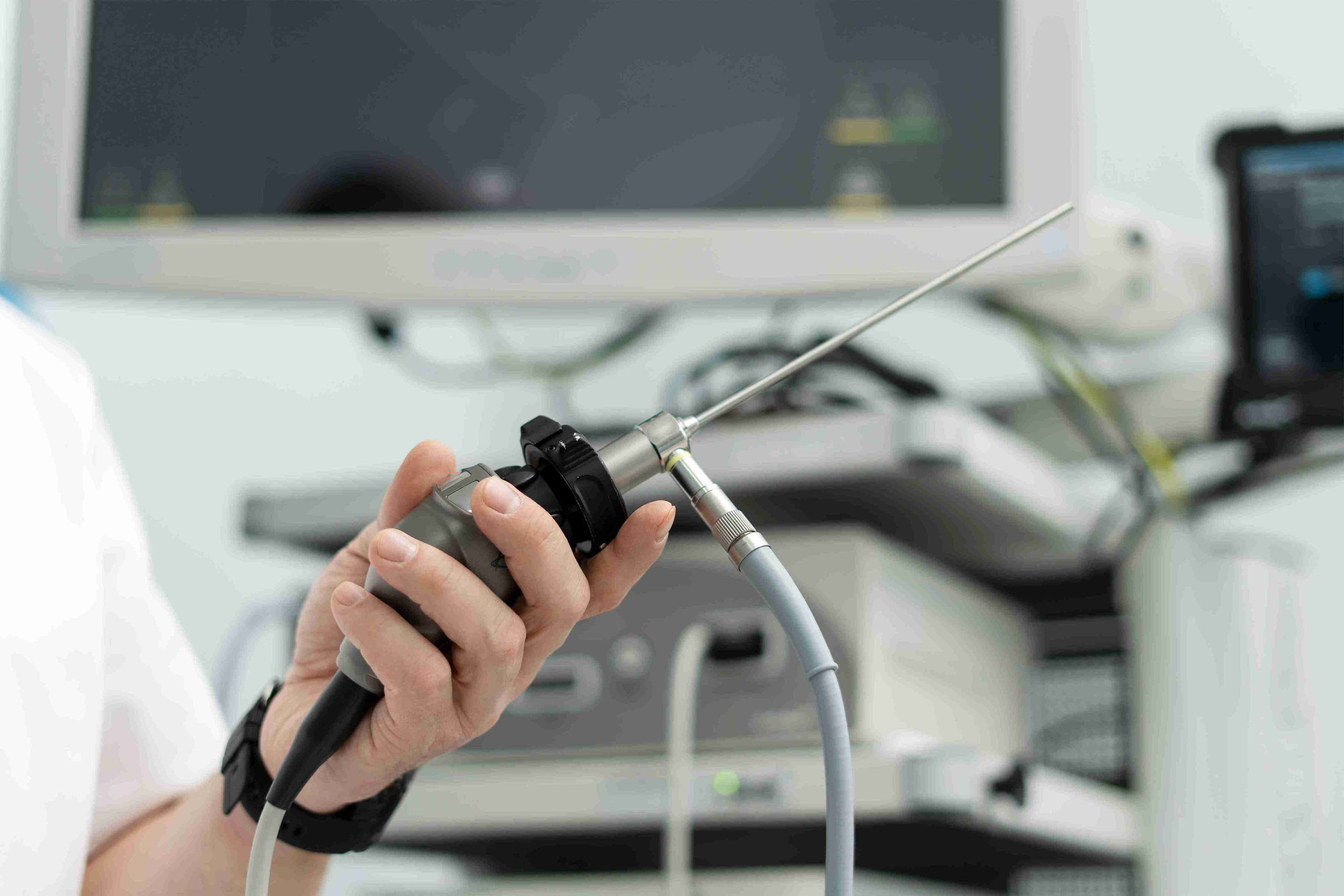
Before diving into the specifics of upper and lower endoscopy, it’s essential to understand the role of endoscopy itself. Endoscopy is a procedure that uses a thin, flexible tube with a light and camera (called an endoscope) to examine the inside of the body. It is commonly used to assess the gastrointestinal (GI) tract, but it can also be used for other areas like the respiratory system or urinary tract.
Both upper and lower endoscopies are outpatient procedures and are generally well-tolerated. They are used for diagnostic purposes but can also be therapeutic in nature, such as removing growths or taking tissue samples for biopsy.
What is Upper Endoscopy?
Upper endoscopy, or esophagogastroduodenoscopy (EGD), is used to examine the upper part of the digestive system, including the esophagus, stomach, and the first part of the small intestine (duodenum). This procedure is typically recommended when a patient has symptoms related to the upper GI tract, such as:
- Persistent abdominal pain
- Difficulty swallowing (dysphagia)
- Heartburn or acid reflux
- Unexplained weight loss
- Bleeding from the gastrointestinal tract (e.g., vomiting blood or black stools)
- Vomiting or nausea
During the procedure, the patient is usually sedated, and the endoscope is inserted through the mouth and gently advanced down the throat. The physician can then visually inspect the esophagus, stomach, and duodenum, and take biopsies if necessary.
Conditions detected by upper endoscopy include:
- Gastroesophageal reflux disease (GERD)
- Peptic ulcers
- Infections (e.g., H. pylori)
- Inflammatory conditions (e.g., gastritis)
- Tumors or cancer
- Celiac disease
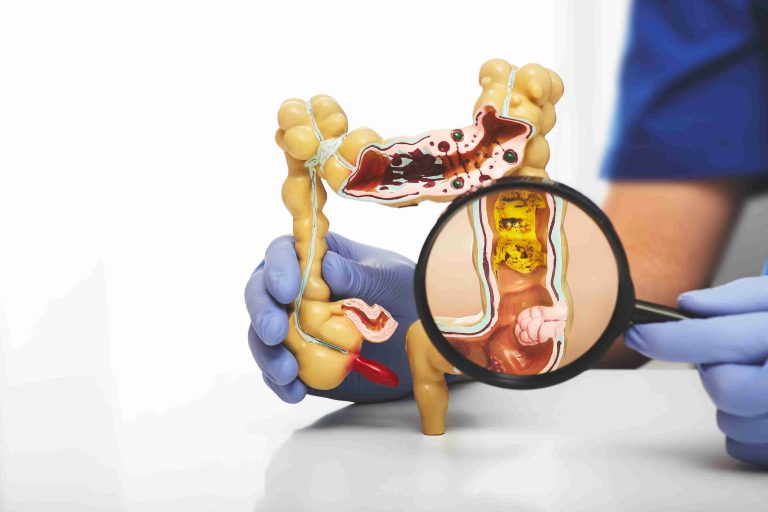
What is Lower Endoscopy?
Lower endoscopy, or colonoscopy, focuses on the lower part of the digestive system, specifically the colon (large intestine) and rectum. This procedure is recommended for individuals experiencing symptoms like:
- Abdominal pain or cramping
- Persistent changes in bowel habits (e.g., diarrhea, constipation)
- Blood in stools
- Unexplained weight loss
- Family history of colorectal cancer or polyps
- Screening for colorectal cancer (typically starting at age 50)
During a colonoscopy, the endoscope is inserted through the rectum and advanced through the colon. The patient is typically sedated for comfort, and the procedure lasts around 30 minutes to an hour. As with upper endoscopy, biopsies can be taken, and polyps or other growths can be removed during the procedure.
Conditions detected by lower endoscopy include:
- Colon polyps (which can be precursors to colorectal cancer)
- Inflammatory bowel diseases (e.g., Crohn’s disease, ulcerative colitis)
- Colorectal cancer
- Diverticulosis or diverticulitis
- Gastrointestinal bleeding or inflammation
Key Differences Between Upper and Lower Endoscopy
While both upper and lower endoscopies are used to examine different sections of the gastrointestinal tract, several factors distinguish these procedures from each other.
1. Area of Focus
The most apparent difference is the area of the body they examine. Upper endoscopy focuses on the upper GI tract, while lower endoscopy examines the lower GI tract. This distinction is essential for diagnosing conditions that affect each area.
2. Symptoms and Conditions
The types of symptoms and conditions prompting each procedure also vary. Upper endoscopy is commonly used for symptoms like difficulty swallowing, heartburn, or unexplained nausea, whereas lower endoscopy is used for issues such as blood in the stool, changes in bowel movements, or abdominal pain.
3. Procedure Process
In terms of procedure, upper endoscopy is performed through the mouth, while lower endoscopy is performed through the rectum. Both procedures are generally done under sedation, although patients may be more familiar with the colonoscopy due to its more widespread use in cancer screening.
4. Preparation
While both procedures require some preparation, the preparation for a lower endoscopy tends to be more involved. For colonoscopy, patients are usually required to follow a clear liquid diet and take laxatives the day before the procedure to ensure the colon is completely clear. On the other hand, upper endoscopy typically requires less preparation, with fasting from food and liquids for a few hours before the procedure.
5. Screening vs. Diagnostic
Lower endoscopy (colonoscopy) is often used as a screening tool for colorectal cancer, while upper endoscopy is generally used for diagnostic purposes when a patient is experiencing symptoms. However, both procedures can be used for diagnostic purposes depending on the individual’s symptoms.
When Are These Procedures Needed?
Both upper and lower endoscopy are valuable in diagnosing gastrointestinal conditions, but the decision to use one over the other is based on a person’s symptoms and medical history.
Upper Endoscopy
- If a patient is experiencing persistent heartburn, difficulty swallowing, or unexplained nausea, upper endoscopy is typically recommended.
- Those with a family history of esophageal or stomach cancer may also be candidates for this procedure.
- People who have symptoms like vomiting blood or passing black stools may need an upper endoscopy to identify the cause of GI bleeding.
Lower Endoscopy
- Those experiencing rectal bleeding, blood in stools, or a change in bowel habits may need lower endoscopy to rule out colorectal cancer or other GI conditions.
- If a patient has a family history of colon polyps or colorectal cancer, they may be advised to undergo colonoscopy screenings starting at age 50 or earlier if there are additional risk factors.
- Individuals with chronic conditions such as inflammatory bowel disease may require regular colonoscopies to monitor their health.
Conclusion
Understanding when an endoscopy is needed and whether an upper or lower endoscopy is appropriate is essential for managing gastrointestinal health. While both procedures are non-invasive and provide valuable insights into the digestive system, they are used for different purposes based on symptoms, medical history, and risk factors.
Upper endoscopy is typically employed to investigate issues in the esophagus, stomach, and duodenum, whereas lower endoscopy is primarily used to examine the colon and rectum. Each procedure plays a critical role in diagnosing conditions such as ulcers, cancer, inflammatory bowel disease, and polyps.