Chronic gastric issues can significantly impact quality of life, and in many cases, they require ongoing monitoring and evaluation. One of the most effective diagnostic tools used in assessing gastrointestinal problems is the endoscopy. But how often should someone with chronic gastric issues undergo this procedure? The answer depends on several factors including the nature of the symptoms, underlying conditions, and risk factors.
What Is an Endoscopy?
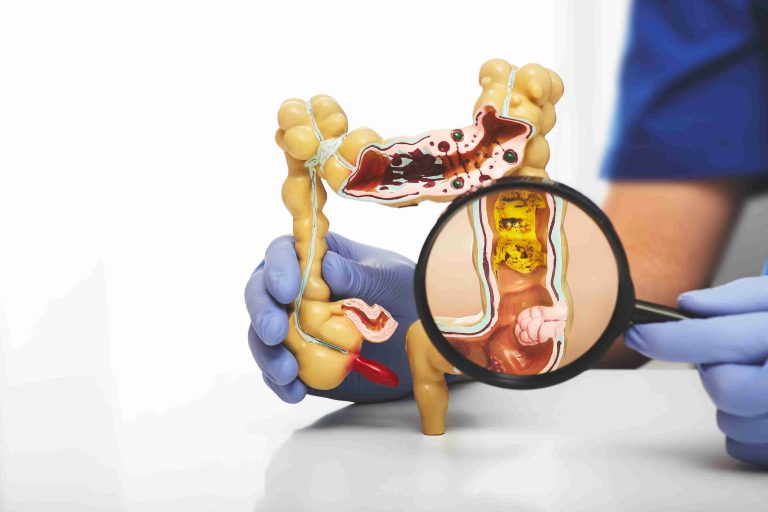
An endoscopy is a procedure that uses a flexible tube with a light and camera attached to it (called an endoscope) to view the inside of the digestive tract. In most cases involving gastric issues, a gastroscopy (or upper endoscopy) is performed to examine the esophagus, stomach, and the first part of the small intestine (duodenum).
This procedure allows doctors to visually inspect the lining of these organs and to take biopsies if needed. It is particularly useful in diagnosing ulcers, gastritis, gastroesophageal reflux disease (GERD), Barrett’s esophagus, and even gastric cancer.
Chronic Gastric Issues That May Require Regular Endoscopies
People suffering from chronic gastric issues may present with a range of symptoms including persistent stomach pain, bloating, nausea, heartburn, vomiting, and unexplained weight loss. Several underlying conditions often necessitate regular endoscopy exams:
- GERD (Gastroesophageal Reflux Disease): In cases where GERD is severe or long-standing, there is a risk of developing Barrett’s esophagus, a condition that can lead to esophageal cancer. Regular monitoring with endoscopy is often recommended.
- Chronic Gastritis: Caused by H. pylori infection, autoimmune issues, or long-term NSAID use, chronic gastritis can lead to complications like ulcers or increased cancer risk, making periodic endoscopic evaluations important.
- Peptic Ulcers: Although ulcers may heal with treatment, some patients experience recurrent symptoms, and endoscopy helps ensure healing and rule out malignancy.
- Barrett’s Esophagus: This condition warrants routine surveillance because of its association with a higher risk of esophageal adenocarcinoma.
- Family or Personal History of GI Cancer: Individuals with a genetic predisposition or previous history of gastrointestinal cancers often undergo regular endoscopies as a precaution.
Frequency of Endoscopy Based on Condition
There is no one-size-fits-all recommendation for how often someone with chronic gastric issues should have an endoscopy. However, medical guidelines and research do provide some general advice depending on the diagnosis.
GERD Without Complications
For patients with mild to moderate GERD and no alarming symptoms (like difficulty swallowing or weight loss), an initial endoscopy may be performed to confirm diagnosis. If symptoms are well-controlled with medication, repeat endoscopy might not be necessary unless symptoms change or worsen.
Barrett’s Esophagus
Surveillance guidelines suggest that people with non-dysplastic Barrett’s esophagus undergo an endoscopy every 3 to 5 years. If low-grade dysplasia is detected, endoscopy may be repeated every 6 to 12 months. In cases of high-grade dysplasia, more frequent exams or treatment options like ablation may be necessary.
Chronic Gastritis and H. pylori Infection
Once H. pylori has been treated and symptoms resolve, many patients won’t need frequent endoscopies. However, if gastritis is persistent or there are concerning features such as intestinal metaplasia or dysplasia, periodic surveillance every 1 to 3 years might be warranted.
Patients with autoimmune gastritis may also require ongoing endoscopy to monitor for changes, particularly if they have other risk factors like anemia or family history of gastric cancer.
Peptic Ulcer Disease
After treatment, a follow-up endoscopy may be needed in 6 to 8 weeks to confirm ulcer healing, particularly in older adults or if the ulcer was bleeding. For uncomplicated ulcers with no worrying features, repeat procedures are often unnecessary unless symptoms recur.
Esophageal or Gastric Cancer Survivors
Patients who have had cancer in the upper gastrointestinal tract often undergo routine endoscopy as part of post-treatment surveillance, typically every 6 to 12 months depending on the type and stage of cancer.
Symptoms That May Warrant an Earlier Endoscopy
Even if your condition doesn’t fall under the high-risk categories, certain symptoms may prompt an earlier or repeat endoscopy, including:
- Sudden or unexplained weight loss
- Difficulty swallowing
- Vomiting blood or black, tarry stools
- Severe or persistent abdominal pain
- Iron-deficiency anemia
- A change in usual gastric symptoms
These symptoms are considered “alarm features” and should never be ignored, as they could signal more serious conditions like bleeding ulcers or gastrointestinal cancers.
Age and Risk Factors Also Matter
Older adults and those with a family history of gastric or esophageal cancer may require more frequent monitoring, even in the absence of severe symptoms. Lifestyle factors such as smoking, alcohol use, and diets high in processed foods may also increase the need for regular evaluations.
In some cases, doctors may recommend endoscopy every few years as a preventive measure in high-risk individuals, even if they’re asymptomatic.
When Is Endoscopy Not Necessary?
It’s important to note that endoscopy is not always the first or most appropriate test for chronic gastric issues. For example, functional dyspepsia (non-ulcer stomach pain) or IBS (irritable bowel syndrome) may not require endoscopic evaluation unless alarm symptoms are present.
In many mild cases, doctors may first recommend lifestyle changes, medications like proton pump inhibitors (PPIs), or non-invasive tests such as breath or stool tests for H. pylori before considering an endoscopy.
Working with Your Doctor to Determine the Right Schedule
Your gastroenterologist will consider many factors before recommending how often you should undergo endoscopy:
- Your diagnosis and symptoms
- The presence of high-risk conditions
- Response to treatment
- Family history and personal health background
It’s essential to maintain open communication and attend regular follow-ups so your care can be tailored appropriately. You should also inform your healthcare provider about any new or worsening symptoms as they develop, even if your last endoscopy was recent.
The Role of Endoscopy in Long-Term Management
While endoscopy is an invasive procedure, it plays a crucial role in both diagnosing and monitoring chronic gastric conditions. The ability to directly visualize the digestive tract and collect biopsies makes it an invaluable tool in preventing disease progression and detecting cancer early.
However, it should be used judiciously and not as a routine test in the absence of clear indications. Overuse can lead to unnecessary risks, while underuse could delay critical diagnoses.
Conclusion
So, how often should you have an endoscopy if you have chronic gastric issues? The answer is highly individual and should be guided by medical advice based on your symptoms, diagnosis, and overall health.
For many, one endoscopy every few years may be sufficient. For others, especially those with Barrett’s esophagus, persistent ulcers, or high cancer risk, more frequent surveillance is necessary.
Understanding your condition, recognizing warning signs, and staying engaged with your healthcare provider are key steps in managing chronic gastric issues effectively.