Colonoscopy screening has long been one of the most reliable methods for detecting colon cancer and other gastrointestinal abnormalities early. It not only helps catch problems before they become serious but also allows doctors to remove precancerous polyps during the procedure itself.
However, like many medical interventions, there comes a time when the benefits of continued screening may no longer outweigh the risks. So how do you know when to stop colonoscopy screening?
The answer isn’t the same for everyone. It depends on factors like age, medical history, life expectancy, and overall health. Understanding when to discontinue this procedure can help you make informed choices about your long-term care.
The Purpose and Benefits of Colonoscopy
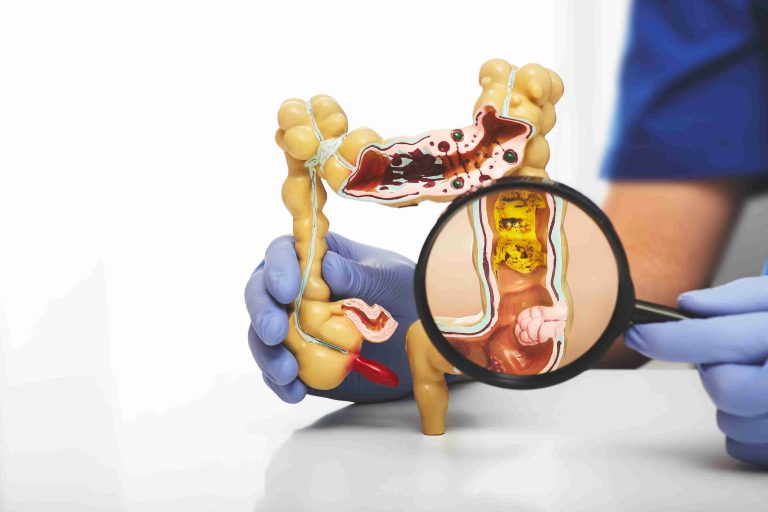
Colonoscopy is typically used to screen for colorectal cancer, a leading cause of cancer-related deaths worldwide. The procedure allows physicians to view the inner lining of the large intestine using a flexible tube with a camera. Any abnormal growths, such as polyps, can be detected and removed during the exam.
For individuals at average risk, colonoscopy screening usually begins at age 45 and is repeated every 10 years if no abnormalities are found. Those with a family history of colorectal cancer, genetic risk factors, or previous findings may need more frequent monitoring.
The primary benefit of colonoscopy is prevention. By detecting and removing polyps before they turn cancerous, the test can dramatically reduce the incidence of colorectal cancer.
When Guidelines Recommend Stopping
Medical guidelines offer general recommendations on when colonoscopy screening should cease, but they also emphasize personalized decision-making.
Most health authorities, including the U.S. Preventive Services Task Force and American Cancer Society, suggest that average-risk adults stop routine colonoscopy screening at age 75. Between ages 76 and 85, the decision becomes more individualized. Beyond age 85, colonoscopy is generally no longer recommended.
These age-based guidelines are rooted in the balance between benefit and risk. As people age, the likelihood of developing new colon cancer decreases, while the risks associated with colonoscopy—such as bleeding, perforation, and complications from sedation—increase.
Evaluating Life Expectancy and Overall Health
Chronological age isn’t the only factor to consider. A more relevant consideration is your overall health status and life expectancy.
If someone is 78 but in excellent health with no significant chronic conditions, they may still benefit from continued colonoscopy screening. On the other hand, a 70-year-old with multiple serious medical issues may face more risk than benefit from undergoing the procedure.
Doctors often use life expectancy tools or consider whether a patient is likely to live at least 10 more years—the approximate period it takes for a precancerous polyp to become cancerous. If a person is not expected to live that long due to unrelated health issues, continuing colonoscopy screening may not improve their quality or length of life.
Past Screening Results Matter
Your previous colonoscopy outcomes also influence the decision to stop. If your most recent screenings have been normal and you don’t have a family history of colon cancer or other risk factors, it’s reasonable to consider stopping around the recommended age.
Conversely, if you’ve had polyps removed in the past or have a personal history of colorectal cancer, your doctor may recommend continuing colonoscopy screening past the age of 75. Surveillance in these cases is more closely tied to personal risk rather than population-based guidelines.
It’s important to maintain a dialogue with your doctor and review your screening history carefully before making any decisions.
Risks of Continuing Colonoscopy in Older Adults
While colonoscopy is generally safe, the risks increase as you get older. Older adults may be more vulnerable to complications related to sedation, bowel preparation, or the procedure itself.
For instance, the prep solution required to clear the bowel can cause dehydration or electrolyte imbalances in elderly patients. Sedation may result in confusion or falls, particularly in those with preexisting cognitive decline or frailty. There’s also a small but real risk of bleeding or bowel perforation during the procedure.
These risks become more relevant as age and comorbidities increase, and they play a crucial role in determining when to stop colonoscopy screening.
Exploring Alternatives and Less Invasive Options
If you’re nearing the recommended age to stop colonoscopy or have concerns about the procedure’s risks, there are less invasive options that might still offer some level of cancer surveillance.
Stool-based tests like the fecal immunochemical test (FIT) or stool DNA tests (like Cologuard) can detect traces of blood or altered DNA that may signal colorectal cancer. These tests are not as comprehensive as a colonoscopy, but they are easier to complete at home and pose no procedural risk.
However, if these tests return abnormal results, a follow-up colonoscopy will still be required. Therefore, these alternatives are often considered interim tools for people unable or unwilling to undergo colonoscopy, rather than complete replacements.
Making an Informed and Individualized Decision
Deciding when to stop colonoscopy screening is a personal and often complex choice. It should be based on a thorough conversation between you and your healthcare provider, weighing your age, overall health, previous screening results, and personal preferences.
Many patients find comfort in creating a plan for when and how they’ll transition away from colonoscopy. For instance, some may decide to stop routine screening at 75 but continue stool-based testing for a few more years. Others might opt to stop all forms of colorectal cancer screening after a certain milestone, such as a decade of clean colonoscopies.
Your doctor can help you navigate this decision by reviewing your health records, explaining the pros and cons, and tailoring a plan to your specific situation.
The Importance of Monitoring Symptoms at Any Age
Even if you’ve stopped colonoscopy screening, you should remain alert to any new gastrointestinal symptoms. These may include changes in bowel habits, rectal bleeding, abdominal pain, unexplained weight loss, or fatigue.
At any age, the appearance of symptoms like these warrants further evaluation, even if you’re no longer undergoing routine screening. Colonoscopy may still be used as a diagnostic tool rather than a preventive one in such cases.
Colon cancer doesn’t always follow predictable patterns, so staying in tune with your body and communicating with your healthcare provider remains vital throughout your life.
Conclusion
Colonoscopy screening has saved countless lives by detecting colon cancer early and preventing its development through polyp removal. But there comes a point when continuing this screening no longer offers significant benefit, especially if a person’s health is in decline or life expectancy is limited.
By understanding when to stop colonoscopy screening and exploring alternatives, you can approach your health care with clarity and confidence. Most importantly, have ongoing conversations with your doctor to determine the best course of action for your individual needs. Colonoscopy is just one part of a larger health journey, and knowing when to let go of it is part of responsible, informed care.