Key Takeaways
- A traditional colonoscopy remains the most accurate method for detecting and removing colorectal polyps in a single procedure.
- Virtual colonoscopy is less invasive and quicker but cannot treat abnormalities if they are found.
- The right screening option depends on medical risk, patient preference, and the need for definitive diagnosis.
- Understanding the strengths and limitations of each approach helps patients make informed screening decisions.
Colonoscopy vs Virtual Colonoscopy: Which Option Is Better?
Colorectal cancer screening is essential for detecting disease early, when treatment is most effective. Among the available options, a conventional colonoscopy and virtual colonoscopy are often compared. While both evaluate the colon, they differ significantly in methodology, accuracy, and therapeutic capabilities. Understanding these differences is critical for patients deciding on the most appropriate screening strategy.
A traditional colonoscopy allows for immediate diagnosis and treatment, making it ideal for higher-risk individuals or those with a history of polyps. Virtual colonoscopy, in contrast, is less invasive, faster, and may appeal to low-risk individuals or those unable to undergo a standard procedure. Each method has unique benefits and limitations that influence patient choice.
Understanding Colorectal Screening
Screening for colorectal cancer aims to detect precancerous polyps or early-stage cancer before symptoms develop. Early detection greatly improves prognosis and allows for less invasive treatment. Several screening methods exist, including stool-based tests, flexible sigmoidoscopy, colonoscopy, and virtual colonoscopy.
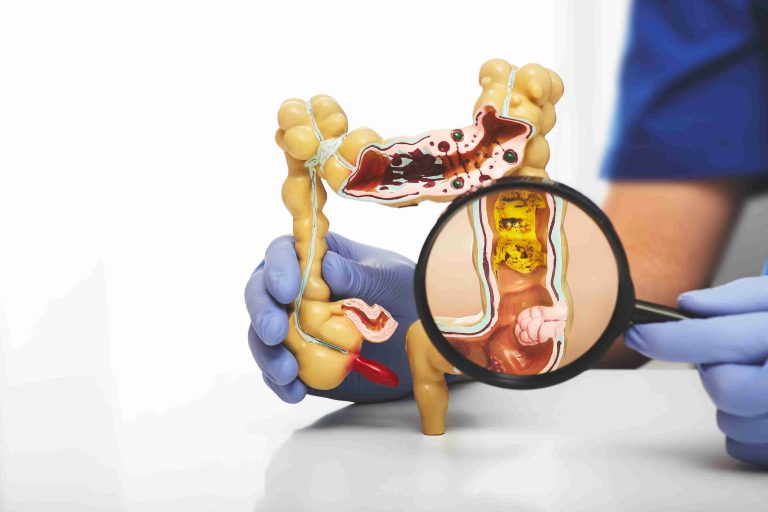
Among these, colonoscopy and virtual colonoscopy are frequently discussed together because both visualize the colon in detail. While a conventional colonoscopy provides direct inspection, biopsy, and polyp removal, virtual colonoscopy relies on advanced imaging to create a “virtual” view of the colon lining. The choice between these methods depends on clinical risk factors, patient comfort, and the need for immediate intervention.
What Is a Traditional Colonoscopy?
Traditional colonoscopy uses a flexible tube with a camera (colonoscope) to examine the entire colon. Typically performed under sedation, the procedure ensures patient comfort while allowing the gastroenterologist to observe the intestinal lining directly.
One of the key advantages of colonoscopy is its therapeutic capability. If polyps or suspicious lesions are found, they can be removed immediately during the same session. Biopsies can also be taken for further laboratory analysis, ensuring that potentially precancerous changes are addressed promptly.
Colonoscopy is considered the gold standard in colorectal screening due to its high sensitivity and specificity. Small lesions, flat polyps, and subtle mucosal abnormalities that imaging may miss can be identified and treated in a single procedure. This dual diagnostic and therapeutic function makes colonoscopy the preferred method for high-risk patients or those with symptoms such as rectal bleeding, unexplained anemia, or persistent bowel changes.
What Is Virtual Colonoscopy?
Virtual colonoscopy, also known as CT colonography, uses computed tomography to create detailed images of the colon. Unlike conventional colonoscopy, it does not require inserting a scope throughout the colon, making it a less invasive option.
The procedure is usually quicker than a traditional colonoscopy and does not require sedation, allowing patients to resume daily activities almost immediately. Virtual colonoscopy is particularly appealing for individuals who may be anxious about invasive procedures or those with medical conditions that make sedation risky.
However, virtual colonoscopy is purely diagnostic. If abnormalities such as polyps or tumors are detected, a follow-up colonoscopy is required to confirm the findings and perform treatment. This two-step approach can impact cost, convenience, and overall screening strategy.
Accuracy and Diagnostic Capability
Traditional colonoscopy remains the most accurate method for detecting colorectal polyps, early cancers, and subtle mucosal changes. Direct visualization allows clinicians to identify even small or flat lesions that might be missed by imaging alone. The ability to perform polypectomy during the same session enhances its preventive value.
Virtual colonoscopy is effective at detecting larger polyps and masses but may miss smaller lesions. Its sensitivity for detecting polyps less than 6 mm is lower than conventional colonoscopy. Consequently, patients with abnormal findings will need a standard colonoscopy to confirm results and allow treatment, which may lead to additional preparation and procedural time.
Preparation and Patient Experience
Both colonoscopy and virtual colonoscopy require thorough bowel preparation. Cleansing the colon ensures clear visualization and accurate detection of abnormalities. Many patients cite the bowel prep as the most uncomfortable part of the screening process.
During colonoscopy, sedation helps minimize discomfort, but patients require a companion to escort them home. In contrast, virtual colonoscopy avoids sedation, which allows patients to resume normal activities immediately after the scan. Some patients may prefer this aspect, particularly if they have responsibilities or travel constraints.
Safety and Risk Considerations
Colonoscopy is generally safe but carries small procedural risks, including bleeding or bowel perforation, particularly during polyp removal. Complications are rare when performed by experienced specialists in accredited facilities.
Virtual colonoscopy avoids these procedural risks because no instruments are inserted into the colon. However, it involves exposure to a low dose of ionizing radiation, which may be a consideration for some patients, particularly those requiring repeated imaging over time. Understanding these risks is essential for informed decision-making.
Suitability Based on Risk Profile
For individuals at average risk with no symptoms, virtual colonoscopy may be an acceptable screening option. It is a convenient, non-invasive method for initial evaluation and can detect larger polyps or masses effectively.
Patients with a higher risk of colorectal cancer—such as those with a family history, previous polyps, or chronic inflammatory bowel disease—are generally advised to undergo traditional colonoscopy. This approach ensures that any abnormalities can be addressed immediately, reducing the need for multiple procedures and optimizing preventive care.
Follow-Up and Long-Term Planning
Screening frequency depends on risk factors and findings. A normal colonoscopy may not need to be repeated for 10 years, whereas abnormal results or polyp removal may necessitate more frequent follow-up.
Virtual colonoscopy, being diagnostic only, may require earlier repetition, especially if risk factors are present. Any positive finding requires subsequent colonoscopy, adding an additional step in long-term screening planning. These considerations can influence patient preference and overall efficiency.
Cost, Access, and Practical Factors
Cost and availability vary by region and healthcare system. Virtual colonoscopy is often more accessible and appealing for those unable to tolerate sedation. However, when considering the potential need for follow-up colonoscopy, traditional colonoscopy may be more cost-effective in the long term for patients likely to require intervention.
Insurance coverage, Medisave eligibility, and institutional policies also affect out-of-pocket expenses. Discussing these factors with a healthcare provider ensures transparency and helps patients make informed financial decisions.
Making the Right Choice With Your Doctor
Choosing between colonoscopy and virtual colonoscopy should be a shared decision. Patients should discuss their age, medical history, family history, comfort level with procedures, and overall risk factors with their healthcare provider.
An open discussion ensures that the screening method aligns with both medical needs and personal preferences. It also allows patients to weigh factors such as accuracy, convenience, potential follow-up procedures, and cost.
Conclusion
Both colonoscopy and virtual colonoscopy have distinct advantages and limitations. Virtual colonoscopy offers convenience, minimal invasiveness, and quick recovery, making it a suitable choice for low-risk individuals. Traditional colonoscopy, however, provides definitive diagnosis and immediate treatment, making it the gold standard for high-risk patients or those requiring therapeutic intervention.
By understanding the pros and cons of each method, patients can take an active role in colorectal health, ensuring timely screening and better long-term outcomes. Ultimately, the choice should balance medical accuracy, safety, patient comfort, and practical considerations to optimize preventive care and early detection of colorectal disease.